- Area: Quality of life
- Start date: September 2021
- End date: Noviembre 2021
- Links:
- Type: MCIN/AEI y FEDER
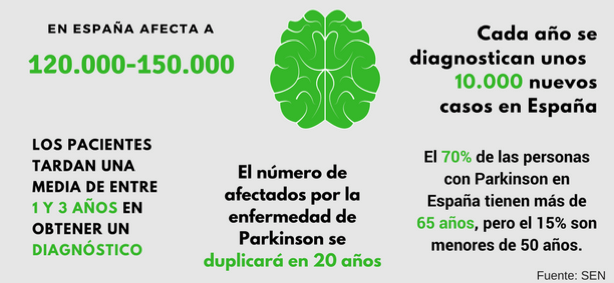
According to Sociedad Española de Neurología (SEN), Parkinson’s disease prevalence and incidence is increasing and estimated that the number of people affected will double in 20 years and triple in 2050. Following figure illustrate main issues behind the disease being the second most frequent neurological diagnosis among those over 65.
This project addresses a new research line that aims to use data generated from smart insoles to objectively support an early treatment of Parkinson disease (PD) and consequently improve the life quality of patients. Three research groups with extensive experience in this field and with complementary scientific expertise bring forces together in this project: ISI (UPC), HOWLAB (UZ) y B105 (UPM).
The project’s hypothesis and objectives are the framework of Maria’s story, a 58-years old person who lives with his husband, Alfonso, and their teenage son, Diego. She works as a pharmacist and suffers from Parkinson disease. She enjoys jogging and practising yoga in her free time. Since she experienced the first symptoms of PD, she started a treatment with a physiotherapist, who also prescribed her exercises that she practices every day. She also visits her neurologist every 6 months to follow up her evolution and check if medication is working well. Both her physiotherapist and her neurologist can access the data provided by the smart insoles she is wearing. The data is provided by key parameters and their historical record, in case the health professionals want to check the changes from previous periods of time. Also, a ready-to-use report is available that integrates all the changes and the evolution between two periods of time, allowing the health professionals to save time during their clinical assessment and focus on the main relevant changes that have taken place. Currently, she is starting to suffer FOG episodes, but she stills feels confident of walking on her own, because when the smart insoles detect this problem, they apply a rhythmic vibration (only perceptible for her) that allows her to get over and continue walking (without the typical paralysis that makes her feel so powerless). Her husband is also able to keep his lifestyle, and goes to work without worries because he knows that if her wife -who still wants to be autonomous when alone at their home- suffers a fall, the system will call him automatically (falls are the primary etiology of accidental deaths in elderly, and early detection exponentially reduces mortality), allowing her to receive quick attention.
Cristian is Maria´s physiotherapist. He treats Maria on a daily basis according to the approved protocol for PD patients in the Aragon Parkinson Association. However, he feels that he is unable to accurately customize the treatment for each patient. When he tries to increase the intensity of the exercises to be sufficiently demanding and challenging for the patients -which is the basis of improvement- the risk of fatigue and falls also increases. Besides, everyday Cristian asks their patients about how they feel in order to adapt the intensity or the workload. Having more objective information for everyday treatment would help him to maximize the treatment effects.
Sara is Maria’s neurologist. She has been working in a public hospital for fifteen years. Many years ago, and although she enjoys both medicine and direct contact with their patients, her work has become overwhelming. With only a few minutes available for each patient, she had to interpret the pieces of information the patient or family tried to explain (with more or less success), to deduce if the last medication she prescribed is doing well or not and to decide the changes in medication until the next visit. Often, it was a trial and error process, where trials were separated for more than 6 months, too much time in case of an error. Besides, she did not have access to the patient’s evolution until the next visit except when there was a major problem that led to an anticipated consultation. Now, since she uses the smart insoles as a tool with her patients, her professional performance has extremely improved. She can check how the medication prescribed has been working to take decisions based on objective data, ready to use it clinically. Besides, in case that there is a significant variation of gait parameters, she will receive an alert to decide if a change of medication should be prescribed. In this way she can manage her appointments depending on the status of her patients, that is, carrying on an intelligent and efficient appointment management: she can now see her patients in order of priority and with a duration directly proportional to the needs of each patient. In addition, the sensors detect slight changes impossible to detect by humans, so now she can prevent and adapt the medication much earlier and much better than before. Thanks to the smart insoles, she is now offering a much more personalized, better, safest, and closest service. She has also improved her quality of work life and has got her taste for her job back again.
To achieve these common objectives the project is divided into two sub-projects with complementary objectives. In the first one (MyGait_Bio) the measurement systems to obtain BCG and IPG signals will be designed and the signal processing will be developed to reduce the influence of the movement artifacts and to be able to extract all the cardiovascular information from the patient. The system for recharging the batteries of the smart insole based on inductive methods will also be designed. This platform will combine inductive battery recharging with the reading of measurement data stored in the memory of the measurement system.
In the second sub-project (MyGait_Sensors) the aim is to develop intelligent insoles that will allow, by means of force and inertial sensors and advanced algorithms, to monitor the patient’s gait and provide personalised information on the patient’s evolution. This second project also aims to realize experimental tests with clinical supervision that will validate the technologic systems developed and obtain the maximum clinical information.
In this context, the project’s main hypothesis is: The use of a smart insole, able to measure force and movement to characterize the gait and ballistocardiogram (BCG) or the impedance plethysmogram (IPG) to estimate a PD patient’s cardiovascular status variability, can provide objective data about the patient’s evolution to aid clinicians provide a more personalized and effective treatment of PD and consequently improve the patients’ quality of life.
Grant PID2020-116011RB-C22 funded by:

